Renal Physiology
Renal Physiology:
- The actions of the kidney
- Location, structure and function
- Blood supply
- Nephrons
- The glomerulus and peritubular capillaries, the renal tubule.
- Processes
The actions of the kidney
- Maintains purity and constancy of internal fluids
- Regulates blood pressure, volume and chemistry
- Excretion of wastes, toxins and drugs
 - Maintains ion and pH status
- Maintains ion and pH status- Stimulates production of red blood cells
- Calcium absorption
 | |
| Blood Supply |

Blood supply: 20-25% of cardiac output
Blood runs this way:
Renal Artery -> Segmental Arteries -> Interlobar arteries -> Arcuate arteries -> Interlobular arteries -> Afferent-Efferent arterioles -> Peritubular capillaries
Peritubular Capillaries
 - Low pressure porous vessels
- Low pressure porous vessels- Adapted for absorption
- Receive soluts and water from tubule cells
- Drain into interlobular veins leaving the cortex

Nephrons and Urine formation
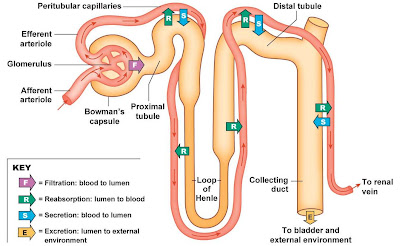
Structural and functional units. Approximately 1 million nephrons per kidney. Two types: cortical and juxta-medullary. Specific regions specialised to perform different functions. Filtration, reabsorption, secretion, excretion
Renal tubule:
- Proximal convoluted tubule (PCT) consists of cuboidal epithelial cells with microvilli that facilitates reabsorption of water and nutrients.
- Loop of Henle (LOH): the first part that dips into medulla ( the descending limb) and first part of ascending limb; consist of squamous epithelium second part of AL is cuboidal.
- Distal convoluted tubule (DCT): in cortex, highly convoluted makes contact with blood in Glomerulus here specialised cells from the Macula densa.
- Collecting duct (CD): empty contents into papillary ducts
DCT and CD: cuboidal cells-principal cells-affected by Vasopressin and Aldosterone.intercalated cells secrete H+ ions
Glomerular (Bowmans) capsule
- water and most solutes filter from blood plasma into the Bowmans space by FILTRATION
- endothelium: capillaries have fenestrations (pores) that restrict passage of blood cells.
- Basement membrane restricts passage of large proteins.
- Podocytes: specialized epithelial cells contain pedicels, filtration slits, slit membranes (prevent passage of medium sized proteins)
[[- Double walled epithelial cup that surrounds the glomerulus.
- Parietal layer separate from visceral layer by the Bowmans space
- Epithelial cells of visceral layer called podocytes with footlike extensions called pedicels]]
Blood pressure
Neural regulation
 |
| Renin-Angiotensin-Aldosterone system |
- Renin release from JGA also stimulated
Hormonal regulation
Low aterial blood pressure triggers release of Renin from JGA that causes:
- Activation of Angiotensin II
- Dilation/Constriction of afferent/efferent arterioles
- Aldosterone release increases reabsorption of Na and water by collecting ducts
- Stimulation of thirst
- Vasopressing release increases water reabsorption by the collecting ducts Regulation of urine concentration and volume
- A critical function of the kidney is to maintain the solute concentration of body fluids at a constant of 300mOsm
- Water accounts for 95% of total volume or urine.
- 5% is organic or inorganic solutes
Mechanisms:
- Passive processes: diffusion, fascilitated diffusion and osmosis
- Active processes: primary and secondary active transport and pinocytosis
Tubular Reabsorption
- 99% of filtrate (178.5 L/day) reabsorbed
- Tmax: maximum amount of substance that can be reabsorbed per minute
- Renal threshold: plasma concentration of substance that exceeds Tmax
Proximal convoluted Tubule (PCT)
- Most of nutrient and water reabsorption. Water uses osmotic gradient created by Na+ reabsorption. Nutrients use Na+ symporters. Wastes partially reabsorbed
Loop of Henle
- Descending limb mainly only permeable to water by osmosis
- Ascending limb mainly only permeable to solutes - Na+,K+, Cl- by symport
Distal convoluted tubule and Collecting duct
- Na+ and Cl- symport
- Water reabsorbed by osmosis
- HCO3- formed in intercalated cells reabsorbed
- H+ secreted by active transport
Urine concentration
- Concentration of urine determined by the amount of water reabsorbed from the later DCT and CD.
- Principal cell permeability controlled by Vasopressin that increases permeability of principal cells to water.
- When Vasopressin is absent dilute urine is therefore formed. When Vasopressin concentration is high, concentrated urine is formed.
Summary
Kidney: maintains purity, constancy of internal fluids. Regulates blood volume and chemistry. Excretion of wastes, toxins and drugs. Outer Cortex and Medullary pyramids. Rich blood supply (1/4 of cardiac output). Nephrons. Processes.
Water Balance
 |
| Water Balance |
The kidneys conserve volume but cannot replace lost volume
Homeostasis of water balance
Water makes up to 45-75% of total body weight. Younger people have more body water. More fat means less water. Water accounts for 60% in females and 55% in males
Fluid intake
Daily water gain is ~2500ml/day. Preformed water: 1600+700=2300ml/day
Metabolic water:
200ml/day
Fluid output
Loss of body water: normally loss equals gain so body maintains constant volume
Kidneys: 1500ml/day; Skin: 500ml/day (400ml evaporates); Lungs: 300ml/day; GIT: 200ml/day
Dehydration
- Stimulation of thirst.
- When water loss is greater than gain resulting dehydration stimulates the thirst centre in the hypothalamus.
- Decreased saliva flow
- Increased blood osmotic pressure
- Decreased blood volume
 | |
| Fluid and Electrolyte homeostasis |
Fluid and Electrolyte homeostasis
The body's integrated responses to changes in blood volume and blood pressure
 |
| Sodium Balance: Homeostatic responses to salt ingestion |
 |
| Sodium Balance: Decreased blood pressure stimulates renin secretion |
 |
| Acid-Base Balance: Hydrogen Ion and pH balance in the body |
Acid-Base Balance:
- Normal pH of plasma is 7.38-7.42.
- H+ concentration is closely regulated; changes can alter tertiary structure of proteins
- Abnormal pH affects the nervous system; acidosis: neurons become less excitable and CNS depression and alkalosis: hyperexcitable
- pH disturbances: associated with K+ disturbances
 |
| Disturbances in Volume and Osmolarity |
Endocrine control of water balance
- Typical daily water fluxes
- Control of water losses - role of ADH
- Control of ADH secretion
- Role of thirst
- Dehydration and the elderly
Water Balance
- Water in - Water out = 0
- Typical daily amounts
- In-regulated by thirst:
Drink 1200ml/day; food 1000; metabolism 350 = total 2550ml/day
- Out - control is through urine output via ADH:
Insensible loss (skin and lungs) 900ml/day; sweat 50; faeces 100, urine 1500 = total 2550ml/day
- Range of urine output <500ml to 20L +
Regulation of Water Loss
- ADH main regulator of short term water loss.
- Small peptide (9aa) from neurohypophysis.
- Administer ADH: low urine volume and high concentration
- Lack of ADH: diabetes insipidus - massive flow dilute urine
- Dehydration: need increased water intake
Actions of ADH
- ADH increases permeability of collecting ducts to water
- So get increased reabsorption of water
- So less water goes to the bladder - antidiuresis
Thirst
Reduced fluid volume and/or Increased extracellular fluid concentration --->> THIRST- Thirst centres in hypothalamus near supra optic nucleus
- Lesion centres -> abolish thirst
- Stimulate centres -> drink
- Osmoreceptors and volume receptors as for ADH
Ageing and Water Balance
Maximum water conservation: young adult urine is 4 x concentrated of plasma (500ml/day)Water loading: urine 10x more diluted than plasma
Both capabilites decline with age
Elderly are more prone to dehydration
Reduced ability to concentrate urine. Decline in thirst acuity - less thirsty at given level dehydration. Less able to get drinks. Voluntary suppression (fear of incontinence)
Consequences: constipation, confusion, increased risk of genito-urinary infections
Daily Salt Balance
Average UK intake is approximately 9g/day
Output: sweat 0.25g/day, faeces 0.25g/day and urine 8.5g/day (24h urine output used to measure daily intake)
Sources UK salt: Natural 10% Table 9% Cooking 6% Processing 75%
World range of intakes <1g-25g/day
Aldosterone
A steroid hormone from zona glomerulosa of the adrenal cortex. A ''salt-retaining hormone'' it reduces sodium content of urine and swear and increases intestinal absorption. It induces the synthesis of proteins involved in sodium transport in target tissues.
Kidney
Aldosterone acts on collecting ducts to increase sodium reabsorption which leads on increased chloride reabsorption (sodium chloride), increased potassium excretion (Na/K pump) and increased water
Most salt is reabsorbed earlier but few % (say 35g) reabsorption dependent on aldosterone:
no aldosterone - all is excreted; very high aldosterone - all retained
Normally amount excreted controlled to reflect intake to achieve salt balance
Too much aldosterone (e.g. primary aldosteronism)
Excess salt retention
Excess water retention
Increased BP and oedema
Excess potassium loss
Excess H+ loss - alkalosis
Too little aldosterone - aldrenalectomy
Excess salt loss
Excess fluid loss
Reduced blood volume (circulatory collapse and death)
What controls aldosterone secretion?
All of the following increase aldosterone secretion:
- Salt depletion
- Reduced blood volume
- Increased plasma potassium
Mechanisms of aldosterone output regulation
1) Nervous mechanism - cut adrenal nerves (''no'' effect)
2) ACTH - corticotrophin rlatively small effect on aldosterone output
3) Direct sensitivity of zona glomerulosa cells to potassium concentration - increased K+ leads to rise in aldosterone
4) Removal of kidneys - decrease in aldosterone
Kidney extract - increase aldosterone
=> Renal factor involved in control of aldosterone release










This is really quite good. Thank you!
ReplyDelete