An Overview
Why do
we eat?
Consider for a
moment a Big Mac. The purpose in your eating a Big Mac, other than simple
hedonism, is to assimilate the nutrients it represents and make them available
to build, repair and maintain your own tissues, as well as provide energy for
studying and occasional other pursuits.
You may have
asked yourself - "Exactly what nutrients are present in a Big Mac that
I can assimilate?" MacDonald's comes close to full disclosure in this regard, but what they
don't tell you is that in order to take advantage of these nutrients, you have
to provide the means to carefully break them down into much smaller molecules
that can be imported into blood. Luckily, your digestive system takes care of
this very complex process so efficiently that most of the time you don't even
need to think about it.
At its
simplest, the digestive system it is a tube running from mouth to anus. This
tube is like an assembly line, or more properly, a disassembly line. Its chief
goal is to break down huge macromolecules (proteins, fats and starch), which
cannot be absorbed intact, into smaller molecules (amino acids, fatty acids and
glucose) that can be absorbed across the wall of the tube, and into the
circulatory system for dissemination around your body.
The breakdown of
foodstuffs like a Big Mac is accomplished through a combination of mechanical
and enzymatic processes. To accomplish this breakdown, the digestive tube
requires considerable assistance from accessory digestive organs such as the
salivary glands, liver and pancreas, which dump their secretions into the tube.
The name "accessory" should not be taken to mean dispensable; indeed,
without pancreatic enzymes you would starve to death in short order.
In many ways,
the digestive system can be thought of as a well-run factory in which a large
number of complex tasks are performed. The three fundamental processes that
take place are:
Secretion: Delivery of enzymes,
mucus, ions and the like into the lumen, and hormones into blood.
Absorption: Transport of water, ions
and nutrients from the lumen, across the epithelium and into blood.
Motility: Contractions of smooth
muscle in the wall of the tube that crush, mix and propel its contents.
Each part of
the digestive tube performs at least some of these tasks, and different regions
of the tube have unique and important specializations.
Like any
well-run factory, proper function of the digestive system requires robust
control systems. Control systems must facilitate communication among different
sections of the digestive tract (i.e. control on the factory floor), and
between the digestive tract and the brain (i.e. between workers and
management). Control of digestive function is achieved through a combination of
electrical and hormonal messages which originate either within the digestive
system's own nervous and endocrine systems, as well as from the central nervous
system and from endocrine organs such as the adrenal gland. Different parts of
these systems are constantly talking to one another. The basic messages are along
the lines of "I just received an extraordinary load of food, so I
suggest you get prepared" (stomach to large intestine) or "For
goodness sake, please slow down until I can catch up with what you've already
given me" (small intestine to stomach).
Finally, a note
about differences in digestive anatomy and physiology among animals. The
digestive systems of humans, dogs, mice, horses, kangaroos and great white
sharks are, to a first approximation, virtually identical. If you look more
carefully however, it becomes apparent that each of these species has evolved
certain digestive specializations that have allowed it to adapt to a particular
diet.
These
differences become particularly apparent when you compare a carnivore like a
dog with a herbivore like a goat or a horse. Goats and horses evolved from
ancestors that subsisted on plants and adapted parts of their digestive tracts
into massive fermentation vats which enabled them efficiently utilize
cellulose, the major carbohydrate of plants.
In contrast, dogs
evolved from animals that lived on the carcasses of other animals, and have
digestive systems that reflect this history - extremely small fermentation vats
and essentially no ability to utilize cellulose. Bridging the gap between
carnivores and herbivores are omnivores like humans and pigs, whose digestive
tracts attest to a historical diet that included both plants and animals.
Digestive Tube Anatomy
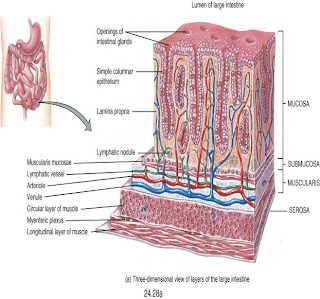
Remarkably
diverse and specialized processes take place in different sections of the
digestive tract, but there is a fundamental consistency in the architecture of
the tubular digestive tract. From the mouth to the anus, the wall of the
digestive tube is composed of four basic layers or tunics.
Tunica serosa is the outermost covering of the digestive tube. In most of the digestive tract (stomach and intestines) it consists of a thin layer of loose connective tissue covered by mesothelium (a type of squamous epithelium that lines body cavities); within the peritoneal cavity, this structure is also referred to as visceral peritoneum.
In the abdominal cavity, the serosa on each side of the tube fuses together to form a suspensory structure called mesentery, which houses vascular and nervous supplies to the digestive tract and is continuous with the lining of the cavity. In regions outside of the abdominal cavity where the digestive tube is essentially affixed to adjacent structures via its outer layer of connective tissue (esophagus and rectum), this tunic is referred to as tunica adventitia instead of tunica serosa.
Tunica muscularis endows the digestive
tube with an ability to be motile. In most of the digestive tube, this
tunic consists of two thick layers of smooth muscle. Muscle fibers in the inner
layer are aligned circularly, whereas those in the outer layer have a
longitudinal orientation.
This combination of circular and longitudinal smooth muscle gives the tube an ability to perform complex movements that squeeze and propel ingesta in the lumen. Between the inner circular and outer longitudinal layers of smooth muscle is another critical component of the digestive tract's nervous system - the myenteric plexus.
This combination of circular and longitudinal smooth muscle gives the tube an ability to perform complex movements that squeeze and propel ingesta in the lumen. Between the inner circular and outer longitudinal layers of smooth muscle is another critical component of the digestive tract's nervous system - the myenteric plexus.
Tunica submucosa, immediately beneath
the mucosa, is a layer of loose to dense connective tissue containing blood and
lymphatic vessels. The submucosa also contains the submucous plexus, a
critical component of the digestive tract's nervous system which provides
nervous control to the mucosa.
Tunica mucosa is the innermost layer of the digestive tube and lines
the lumen. Among the four tunics, the mucosa is most
variable in structure and function, endowing the tube with an ability to
perform diverse and specialized digestive tasks along its length. Of critical
importance in this regard are the epithelial cells that cover the mucosa and
are thus in direct contact with the lumen. This epithelial cell sheet (lamina epithelialis) is distinctly different in different regions of the tract. Indeed, in most of the tract, several different cell types contribute to the epithelium, including cells dedicated to secretion, absorption or production of hormones.
These distinctive differences in architecture of the epithelium can be seen below in the micrographs of mouse digestive tube. The magnification of all four images is identical and the epithelial layer is oriented toward the top.
Beneath the epithelium, but still within the
tunica mucosa is a layer - the lamina propria - of loose connective tissue
through which course blood vessels and lymphatics that supply the epithelium.
This layer also contains lymphatic nodules important to immune functions of the
digestive tract. Finally, beneath the lamina propropria is a thin layer of
smooth muscle ( lamina muscularis mucosae) which permits the mucosa to
dynamically move and fold.
The Digestive System (notes)
•
Gastrointestinal
tract (alimentary canal)
–
mouth
–
pharynx
–
esophagus
–
stomach
–
small
intestine
–
large
intestine
•
Accessory
structures of digestive system
–
teeth
–
tongue
–
salivary
glands
–
liver
–
gallbladder
–
pancreas
Digestive processes
•
Ingestion
–
Taking
of food and liquid into the mouth (eating)
•
Secretion
–
Cells
secrete ~7 litres of fluids per day
•
Mixing
and Propulsion
–
Mixing
and movement of material along GI tract is termed motility
•
Digestion
–
Mechanical
–
Chemical
•
Absorption
•
Defecation
–
Indigestible
material eliminated as feces during defacation
Layers of GI tract
•
Mucosa
–
Epithelium
•
cells
firmly sealed by tight junctions
•
secretes
mucus, digestive enzymes and hormones
•
Absorption
–
Lamina
propria
•
Contains
mucosa-associated lymphatic tissue
–
Muscularis
mucosae
•
causes
folds which increase surface area
•
Submucosa
–
Blood
and lymphatic vessels
–
Glands
–
Submucosal
plexus
•
Regulates
movement of mucosa and vasoconstriction of blood vessels
•
Muscularis
–
Mouth,
pharynx, upper esophagus and external
anal sphincter contain skeletal muscle
–
Rest
of GI tract contains smooth muscle
•
inner
circular and outer longitudinal layers
•
Myenteric
plexus between layers
•
Controls
motility
•
serosa
(visceral peritoneum)
•
Peritoneum
•
Largest
serous membrane in body
–
Parietal
layer
»
Lines
wall of abdomino-pelvic cavity
–
Visceral
layer
»
Covers
some organs in cavity
–
Peritoneal
cavity
»
Contains
serous fluid
Mouth - Salivary glands
•
Mucous
membranes of mouth and tongue secrete small amount of saliva
•
Most
saliva secreted by major salivary glands which lie outside the mouth
–
Parotid
–
Submandibular
Mouth - composition and functions of
saliva
•
Saliva
is ~99.5% water
–
contains:
•
IgA
•
Lysozyme
•
Salivary
amylase
•
Various
solutes, organic substances, etc
•
Saliva
functions to:
–
keep
mucous membranes of mouth and pharynx moist
–
cleanse
mouth and teeth
–
dissolve
food
–
begin
chemical digestion of carbohydrates (salivary amylase)
Mouth - control of salivation
•
Salivation
under nervous control
–
salivary
nuclei in brain stem
•
Receive
input from cortex, taste buds, olfactory apparatus
–
Parasympathetic
output increases salivation
–
Sympathetic
output reduces salivation (dry mouth when stressed)
Mouth – digestion
•
Mechanical
and chemical digestion occur in the mouth
–
Mechanical
digestion results from mastication
–
Chemical
digestion begins
•
Salivary
amylase
–
Initiates
breakdown of starch
•
Lingual
lipase
–
Hydrolyses
triglycerides into fatty acids and glycerol
–
Secreted
in inactive form by glands in tongue
–
Becomes
activated in acid environment of stomach
Pharynx – deglutition
•
Swallowing
occurs in 3 stages:
–
Voluntary
stage
•
Bolus
passed into oropharynx by tongue
–
Pharyngeal
stage
•
Bolus
stimulates stretch receptors in oropharynx
–
Send
impulses to deglutition centre in brain stem
•
Involuntary
passage of bolus into esophagus
–
Esophageal
stage
•
Involuntary
passage of bolus through esophagus into stomach
Esophagus
•
Collapsible
muscular tube behind trachea
–
Secretes
mucus and transports food into stomach
•
Passes
through mediastinum
•
Pierces
diaphragm through esophageal hiatus
•
Upper
and lower sphincters
–
lower
sphincter is physiological sphincter
–
Diaphragm
helps keep lower sphincter closed when not swallowing
•
Food
moves via peristalsis
–
Controlled
by neurons in medulla oblongata
Stomach
–
acts
as a mixing chamber and holding reservoir
–
Starch
digestion continues
–
protein
and triglyceride digestion begins
•
Muscularis
has 3 layers
•
Columns
of secretory cells form gastric glands which line gastric pits
–
Mucous
cells
•
Secrete
mucus
–
Parietal
cells secrete:
•
hydrochloric
acid
•
Intrinsic
factor
•
Required
for absorption of vitamin B12
–
Chief
cells secrete:
•
Pepsinogen
•
Gastric
lipase
–
G
cells
•
Mechanical
digestion
–
After
food enters stomach mixing waves occur every 15-25 sec
•
Aid
in mechanical digestion to form chyme
•
Forces
chyme into duodenum (start of small intestine)
•
Chemical
digestion
–
HCL
•
denatures proteins
–
Pepsinogen
converted to pepsin in presence of HCL and other pepsin molecules
•
Hydrolyses
peptide bonds
–
Gastric
lipase hydrolyses triglycerides
Regulation of gastric secretion and
motility
•
Cephalic
phase
–
Sight,
smell, taste or thought of food
recognised by cerebral cortex or feeding centre in hypothalamus
•
Nerve
impulses sent to medulla oblongata
–
Sends
impulses to submucosal plexus (in submucosa)
»
Increases secretion from
gastric glands and stomach motility (via gastrin secretion)
•
Gastric
phase
–
when
food reaches stomach stimulates
•
Stretch
receptors
•
Chemoreceptors
(monitor pH)
–
Stimulate
secretion of Gastrin (by G cells)
»
Maintains
gastric secretion and motility
•
Intestinal
phase
–
Stimulation
of intestinal receptors as food enters small intestine stimulates secretion of
•
Secretin
– reduces gastric secretion
•
CCK-inhibits
gastric emptying
–
Slows exit of chyme from stomach into duodenum
Pancreas
•
Pancreas
connected to duodenum
–
Secretes
pancreatic juice into duodenum
•
99%
of cells arranged in clusters called acini
–
Exocrine
portion of gland
Pancreas – pancreatic juice
•
Pancreatic
juice contains:
–
Water
–
Salts
–
Sodium
bicarbonate
–
Several
enzymes which digest:
•
carbohydrates
–
Pancreatic
amylase
•
Proteins
–
Trypsin
- secreted in inactive form and activated by brush-border enzyme called
enterokinase
–
Chymotrypsin
– secreted in inactive form and activated by trypsin
–
Cartboxypeptidase
– secreted in inactive form and activated by trypsin
–
Elastase
– secreted in inactive form and activated by trypsin
•
Triglycerides
–
Pancreatic
lipase
•
Nucleic
acids
–
Ribonuclease
–
Deoxyribonuclease
Liver
•
Heaviest
gland in body
•
Two
lobes
–
Large
right lobe
–
Smaller
left lobe
•
Lobes
made up of functional units called lobules
–
Six-sided
structure with hepatocytes arranged around central vein
–
Blood
from hepatic artery and hepatic portal circulation passes through sinusoids and
drains into central veins
–
Bile
enters bile canaliculi and moves to gallbladder
•
Hepatic
artery
–
delivers
oxygenated blood
•
Hepatic
portal circulation
–
delivers
nutrient rich blood from intestines
•
Functions
of liver:
–
CHO
metabolism
•
glycogenolysis
•
gluconeogenesis
•
glycogenesis
–
Lipid
metabolism
•
Synthesise
lipoproteins and cholesterol
•
Store
triglycerides
•
b-oxidation
–
Protein
metabolism
•
Deaminate
amino acids
•
Synthesise
plasma proteins
–
Bile
production
•
Detergent-like
acidic buffer
–
Emulsifies
lipids
–
Process
drugs and hormones
–
Excrete
bilirubin
•
Derived
from heme of worn out RBC (secreted into bile)
–
Store
vitamins and minerals
–
Phagocytosis
of RBC, WBC and bacteria (Kupffer’s cells)
–
Activation
of vitamin D
Gall bladder
•
Bile
production signalled by
•
parasympathetic
activity
•
secretin
- released when acidity in duodenum (secretin also inhibits gastric secretion)
•
Bile
stored and concentrated in gallbladder
–
released
when fatty acids and amino acids enter duodenum
•
signalled
by CCK (also inhibits gastric emptying)
•
Extends
from pyloric sphincter to ileocecal valve
•
3
parts:
–
duodenum
–
jejunum
–
ileum
•
Most
digestion and absorption of nutrients occurs in SI
•
Length
gives large surface area (3m in living person)
–
Surface
area increased by:
•
circular
folds (plicae circulares) - mix chyme
•
villi
- capillaries and lacteals
•
Mechanical
digestion
–
Segmentation
mixes chyme
–
Peristalsis
(migrating motility complex) occurs once absorption complete
•
Slowly
migrates along SI over 90-120 min period
–
Chyme
remains in SI for 3-5 hours
•
Chemical
digestion
–
CHO
•
Pancreatic
amylase splits starch into smaller fragments
•
Brush
border enzyme (a
-dextrinase) then breaks down to glucose
•
Disaccharides
(sucrose, lactose and maltose) broken down by brush border enzymes
–
Proteins
•
Trypsin,
chymotrypsin, carboxypeptidase and elastase break protein down into peptides
•
Each
breaks different peptide bonds
•
Brush
border enzymes aminopeptidase and dipeptidase break peptides into amino acids
–
Lipids
•
Bile
salts emulsify triglycerides into small droplets
•
Pancreatic
lipase hydrolyses triglycerides
–
Nucleic
acids
•
Ribonuclease
and deoxyribonuclease break nucleic acids into nucleotides
•
Brush
border enzymes (nucleosidases and phosphatases) break nucleotides into
pentoses, phosphates and nitrogenous bases
•
Monosaccharides
–
Secondary
active transport with sodium
–
facilitated diffusion (fructose)
•
Amino
acids, dipeptides, tripeptides
–
amino
acids primary or secondary active transport
–
di-
and tripeptides secondary active transport
•
All
move into capillaries in villus
•
Lipids
–
Absorbed
via simple diffusion
•
Others
move into lacteals
–
bile
combines with long-chain fatty acids and monoglycerides to form micelles
•
micelles
contact epithelial cell membrane
•
lipids
diffuse through membrane
•
resynthesised
to triglycerides inside epithelial cells
•
coated
with proteins to form chylomicrons
•
chylomicrons
too large to move into capillaries and move into lacteals
•
Large
molecules (eg complete proteins) not absorbed
–
How
then can foods containing functional proteins exert their effects?
•
eg
bovine colostrum
•
Approx
1.5 m long
•
Extends
from ileocecal sphincter to anus
•
Tonic
contraction of three longitudinal muscles (teniae coli) form pouches (haustra
•
4
divisions:
–
cecum
–
rectum
–
anal
canal
•
internal
sphincter - smooth muscle
•
external
sphincter - skeletal muscle
•
No
villi or circular folds in mucosa
•
Epithelium
contains mostly absorptive cells (water absorption) and goblet cells (secrete
mucus)
•
Mechanical
digestion
–
Movements
of large intestine begin when substances
pass iliocecal sphincter
•
Haustral
churning
•
distention
of haustra as chyme enters LI initiates haustral churning
•
Peristalsis
occurs at slower rate than in SI
•
Mass
peristalsis
•
Strong
peristaltic wave that begins at mid-transverse colon drives contents into
rectum
•
Occurs during or immediately after meal when food
enters stomach
•
Chemical
digestion
–
Final
stage of digestion occurs in LI through activity of bacteria
•
Produces
gases and other by-products
•
Eg
vitamins
Gut – overview
Gut functions – movement/motility, secretion,
digestion, absorption
•
Digestion and absorption of:
–
Carbohydrates
–
Protein
–
Fat
Gut functions
•
Movement/motility, secretion, digestion
absorption
Movement
•
Propulsion of gut contents from mouth to anus
•
Churning and mixing:
–
Hastens dissolving
–
Emulsification
–
Hastens digestion and absorption
Propulsive movements
•
Rhythmic peristaltic waves along gut
•
Constriction of circular muscles behind food
•
Relaxation in front and contraction of
longitudinal muscles
Sphincters
•
Barriers to movement between parts of the gut:
–
Cardiac – oesophagus to stomach
–
Pyloric – stomach to duodenum
–
Ileocaecal – small to large intestine
–
Internal anal – smooth muscle (reflex)
–
External anal – striated muscle (voluntary
control)
Gut secretions
•
Mucous – protects and lubricates whole gut
•
Saliva, Gastric juice, Bile, Pancreatic juice
& Intestinal juice
•
Total 7L/day
Functions gut secretions
•
Dissolve food – allows taste, makes digestible
•
Emulsifies fat
•
Enzymes to digest food
•
Regulates pH and osmolarity
•
Excretion (bile)
•
Fluid, salts and bile salts all largely
reabsorbed
•
Protein of enzymes – digested and absorbed
Control of gut secretion
•
Cephalic – sight, smell, taste – secretion via
nerve stimulation
•
Receptors in gut (mechanical, chemical or osmotic)
via local nerve plexuses or autonomic reflexes stimulate or inhibit glands
•
Endocrine cells in gut respond to stimuli
release hormone into blood which inhibits or stimulates exocrine glands
Digestion
•
Enzymes in gut secretions break down:
–
Starch and disaccharides to monosaccharides
(only these are absorbed)
–
Protein to amino acids, di&tripeptides (also
absorbed along with tiny amount intact protein)
–
Fat (triacylglycerol) monoacylglycerol and fatty
acids
–
DNA & RNA to free mononucleotides
Absorption
•
Large surface area of small intestine – 600X
that of smooth tube
•
Agitation of gut contents speeds absorption
•
Most absorption in duodenum & jejunum
Carbohydrate digestion
•
In the diet:
–
Sucrose and lactose (disaccharides)
–
Amylose (α1-4 links only)
–
Amylopectin (α1-4 and α1-6
links gives very branched chain and makes up most of starch)
–
Other links e.g. β1-4 in cellulose not broken by digestive enzymes but….
•
α-amylase
in saliva & pancreatic juice:
–
Glucose, sucrose, lactose, maltose, maltotriose
and isomaltose
•
On brush border are specific enzymes maltase,
sucrase, lactase and isomaltase
Carbohydrate absorption
•
Glucose and galactose actively absorbed – this
is a carrier-mediated process and is sodium dependent (linked to Na+
pump)
•
Fructose is carrier mediated but not active.
Facilitated diffusion so relatively slow (also things like sorbitol)
Protein digestion
•
Endopeptidases break bonds within protein chain:
–
Stomach – pepsin
–
Intestine –trypsin and chymotrypsin
•
Exopeptidases break of terminal amino acid:
–
Carboxypeptidase in pancreatic juice
–
Aminopeptidases on brush border
•
A range of di&tripeptidases on brush border
Protein absorption
•
Several active carrier mediated processes, some
are Na+ dependent
•
Some di- & tri-peptides absorbed and
digested within mucosal cells
•
Some intact protein absorbed especially in
newborn by pinocytosis – protein toxins, antibodies and passive immunity
Fat digestion/absorption
•
What is fat – triacylglycerol (TAG)?
•
Actions of lipase in vivo – TAG to
monoacylglycerol and 2 fatty acids
•
Fat insoluble in water but pancreatic lipase is
a water soluble enzyme
•
Fat is emulsified by bile salts and
phospholipids
•
Products of fat digestion also low water
solubility
•
Formation of micelles – minute aggregates bile
salts and fat digestion products
•
Absorption by diffusion
•
TAG re-assembled with mucosal cells
•
Chylomicrons formed and enter lymphatic system
then blood (protein coated fat droplets)
•
Chylomicrons lipoprotein lipase in tissue
capillaries breaks fat down to allow absorption and then re-synthesis of TAG
within cells
The GI Immune System
The digestive system is a potential pathogen portal. Large number of bacteria inhabit the gut 1x10^13. The largest immune 'organ' in the body (GI tract) with specialized structures Gut Associated Lymphoid Tissue (GALT). 80% of all lymphocytes are found in the GALT.

Immune cells in Preyers Patches

Immune cells concentrated in

Special epithelial cells called Microfold (M) cells sample the contents of the gut
The GI Protective Responses:
If the immune system is activated then immune cells secrete cytokines. Cytokines trigger inflammatory response and increase Cl-, fluid and mucus secretion.
Diarrhea: immune responses can lead to diarrhea which is an attempt to expel the pathogen. Can lead to dehydration
Vomiting: A protective reflex. Reverse peristalsis along with strong muscular contractions
Crohn's Disease
The Digestive System (notes)
•
Gastrointestinal
tract (alimentary canal)
–
mouth
–
pharynx
–
esophagus
–
stomach
–
small
intestine
–
large
intestine
•
Accessory
structures of digestive system
–
teeth
–
tongue
–
salivary
glands
–
liver
–
gallbladder
–
pancreas
Digestive processes
•
Ingestion
–
Taking
of food and liquid into the mouth (eating)
•
Secretion
–
Cells
secrete ~7 litres of fluids per day
•
Mixing
and Propulsion
–
Mixing
and movement of material along GI tract is termed motility
•
Digestion
–
Mechanical
–
Chemical
•
Absorption
•
Defecation
–
Indigestible
material eliminated as feces during defacation
Layers of GI tract
•
Mucosa
–
Epithelium
•
cells
firmly sealed by tight junctions
•
secretes
mucus, digestive enzymes and hormones
•
Absorption
–
Lamina
propria
•
Contains
mucosa-associated lymphatic tissue
–
Muscularis
mucosae
•
causes
folds which increase surface area
•
Submucosa
–
Blood
and lymphatic vessels
–
Glands
–
Submucosal
plexus
•
Regulates
movement of mucosa and vasoconstriction of blood vessels
•
Muscularis
–
Mouth,
pharynx, upper esophagus and external
anal sphincter contain skeletal muscle
–
Rest
of GI tract contains smooth muscle
•
inner
circular and outer longitudinal layers
•
Myenteric
plexus between layers
•
Controls
motility
•
serosa
(visceral peritoneum)
•
Peritoneum
•
Largest
serous membrane in body
–
Parietal
layer
»
Lines
wall of abdomino-pelvic cavity
–
Visceral
layer
»
Covers
some organs in cavity
–
Peritoneal
cavity
»
Contains
serous fluid
Mouth - Salivary glands
•
Mucous
membranes of mouth and tongue secrete small amount of saliva
•
Most
saliva secreted by major salivary glands which lie outside the mouth
–
Parotid
–
Submandibular
Mouth - composition and functions of
saliva
•
Saliva
is ~99.5% water
–
contains:
•
IgA
•
Lysozyme
•
Salivary
amylase
•
Various
solutes, organic substances, etc
•
Saliva
functions to:
–
keep
mucous membranes of mouth and pharynx moist
–
cleanse
mouth and teeth
–
dissolve
food
–
begin
chemical digestion of carbohydrates (salivary amylase)
Mouth - control of salivation
•
Salivation
under nervous control
–
salivary
nuclei in brain stem
•
Receive
input from cortex, taste buds, olfactory apparatus
–
Parasympathetic
output increases salivation
–
Sympathetic
output reduces salivation (dry mouth when stressed)
Mouth – digestion
•
Mechanical
and chemical digestion occur in the mouth
–
Mechanical
digestion results from mastication
–
Chemical
digestion begins
•
Salivary
amylase
–
Initiates
breakdown of starch
•
Lingual
lipase
–
Hydrolyses
triglycerides into fatty acids and glycerol
–
Secreted
in inactive form by glands in tongue
–
Becomes
activated in acid environment of stomach
Pharynx – deglutition
•
Swallowing
occurs in 3 stages:
–
Voluntary
stage
•
Bolus
passed into oropharynx by tongue
–
Pharyngeal
stage
•
Bolus
stimulates stretch receptors in oropharynx
–
Send
impulses to deglutition centre in brain stem
•
Involuntary
passage of bolus into esophagus
–
Esophageal
stage
•
Involuntary
passage of bolus through esophagus into stomach
Esophagus
•
Collapsible
muscular tube behind trachea
–
Secretes
mucus and transports food into stomach
•
Passes
through mediastinum
•
Pierces
diaphragm through esophageal hiatus
•
Upper
and lower sphincters
–
lower
sphincter is physiological sphincter
–
Diaphragm
helps keep lower sphincter closed when not swallowing
•
Food
moves via peristalsis
–
Controlled
by neurons in medulla oblongata
Stomach
–
acts
as a mixing chamber and holding reservoir
–
Starch
digestion continues
–
protein
and triglyceride digestion begins
•
Muscularis
has 3 layers
•
Columns
of secretory cells form gastric glands which line gastric pits
–
Mucous
cells
•
Secrete
mucus
–
Parietal
cells secrete:
•
hydrochloric
acid
•
Intrinsic
factor
•
Required
for absorption of vitamin B12
–
Chief
cells secrete:
•
Pepsinogen
•
Gastric
lipase
–
G
cells
•
Mechanical
digestion
–
After
food enters stomach mixing waves occur every 15-25 sec
•
Aid
in mechanical digestion to form chyme
•
Forces
chyme into duodenum (start of small intestine)
•
Chemical
digestion
–
HCL
•
denatures proteins
–
Pepsinogen
converted to pepsin in presence of HCL and other pepsin molecules
•
Hydrolyses
peptide bonds
–
Gastric
lipase hydrolyses triglycerides
Regulation of gastric secretion and
motility
•
Cephalic
phase
–
Sight,
smell, taste or thought of food
recognised by cerebral cortex or feeding centre in hypothalamus
•
Nerve
impulses sent to medulla oblongata
–
Sends
impulses to submucosal plexus (in submucosa)
»
Increases secretion from
gastric glands and stomach motility (via gastrin secretion)
•
Gastric
phase
–
when
food reaches stomach stimulates
•
Stretch
receptors
•
Chemoreceptors
(monitor pH)
–
Stimulate
secretion of Gastrin (by G cells)
»
Maintains
gastric secretion and motility
•
Intestinal
phase
–
Stimulation
of intestinal receptors as food enters small intestine stimulates secretion of
•
Secretin
– reduces gastric secretion
•
CCK-inhibits
gastric emptying
–
Slows exit of chyme from stomach into duodenum
Pancreas
•
Pancreas
connected to duodenum
–
Secretes
pancreatic juice into duodenum
•
99%
of cells arranged in clusters called acini
–
Exocrine
portion of gland
Pancreas – pancreatic juice
•
Pancreatic
juice contains:
–
Water
–
Salts
–
Sodium
bicarbonate
–
Several
enzymes which digest:
•
carbohydrates
–
Pancreatic
amylase
•
Proteins
–
Trypsin
- secreted in inactive form and activated by brush-border enzyme called
enterokinase
–
Chymotrypsin
– secreted in inactive form and activated by trypsin
–
Cartboxypeptidase
– secreted in inactive form and activated by trypsin
–
Elastase
– secreted in inactive form and activated by trypsin
•
Triglycerides
–
Pancreatic
lipase
•
Nucleic
acids
–
Ribonuclease
–
Deoxyribonuclease
Liver
•
Heaviest
gland in body
•
Two
lobes
–
Large
right lobe
–
Smaller
left lobe
•
Lobes
made up of functional units called lobules
–
Six-sided
structure with hepatocytes arranged around central vein
–
Blood
from hepatic artery and hepatic portal circulation passes through sinusoids and
drains into central veins
–
Bile
enters bile canaliculi and moves to gallbladder
•
Hepatic
artery
–
delivers
oxygenated blood
•
Hepatic
portal circulation
–
delivers
nutrient rich blood from intestines
•
Functions
of liver:
–
CHO
metabolism
•
glycogenolysis
•
gluconeogenesis
•
glycogenesis
–
Lipid
metabolism
•
Synthesise
lipoproteins and cholesterol
•
Store
triglycerides
•
b-oxidation
–
Protein
metabolism
•
Deaminate
amino acids
•
Synthesise
plasma proteins
–
Bile
production
•
Detergent-like
acidic buffer
–
Emulsifies
lipids
–
Process
drugs and hormones
–
Excrete
bilirubin
•
Derived
from heme of worn out RBC (secreted into bile)
–
Store
vitamins and minerals
–
Phagocytosis
of RBC, WBC and bacteria (Kupffer’s cells)
–
Activation
of vitamin D
Gall bladder
•
Bile
production signalled by
•
parasympathetic
activity
•
secretin
- released when acidity in duodenum (secretin also inhibits gastric secretion)
•
Bile
stored and concentrated in gallbladder
–
released
when fatty acids and amino acids enter duodenum
•
signalled
by CCK (also inhibits gastric emptying)
•
Extends
from pyloric sphincter to ileocecal valve
•
3
parts:
–
duodenum
–
jejunum
–
ileum
•
Most
digestion and absorption of nutrients occurs in SI
•
Length
gives large surface area (3m in living person)
–
Surface
area increased by:
•
circular
folds (plicae circulares) - mix chyme
•
villi
- capillaries and lacteals
•
Mechanical
digestion
–
Segmentation
mixes chyme
–
Peristalsis
(migrating motility complex) occurs once absorption complete
•
Slowly
migrates along SI over 90-120 min period
–
Chyme
remains in SI for 3-5 hours
•
Chemical
digestion
–
CHO
•
Pancreatic
amylase splits starch into smaller fragments
•
Brush
border enzyme (a
-dextrinase) then breaks down to glucose
•
Disaccharides
(sucrose, lactose and maltose) broken down by brush border enzymes
–
Proteins
•
Trypsin,
chymotrypsin, carboxypeptidase and elastase break protein down into peptides
•
Each
breaks different peptide bonds
•
Brush
border enzymes aminopeptidase and dipeptidase break peptides into amino acids
–
Lipids
•
Bile
salts emulsify triglycerides into small droplets
•
Pancreatic
lipase hydrolyses triglycerides
–
Nucleic
acids
•
Ribonuclease
and deoxyribonuclease break nucleic acids into nucleotides
•
Brush
border enzymes (nucleosidases and phosphatases) break nucleotides into
pentoses, phosphates and nitrogenous bases
•
Monosaccharides
–
Secondary
active transport with sodium
–
facilitated diffusion (fructose)
•
Amino
acids, dipeptides, tripeptides
–
amino
acids primary or secondary active transport
–
di-
and tripeptides secondary active transport
•
All
move into capillaries in villus
•
Lipids
–
Absorbed
via simple diffusion
•
Others
move into lacteals
–
bile
combines with long-chain fatty acids and monoglycerides to form micelles
•
micelles
contact epithelial cell membrane
•
lipids
diffuse through membrane
•
resynthesised
to triglycerides inside epithelial cells
•
coated
with proteins to form chylomicrons
•
chylomicrons
too large to move into capillaries and move into lacteals
•
Large
molecules (eg complete proteins) not absorbed
–
How
then can foods containing functional proteins exert their effects?
•
eg
bovine colostrum
•
Approx
1.5 m long
•
Extends
from ileocecal sphincter to anus
•
Tonic
contraction of three longitudinal muscles (teniae coli) form pouches (haustra
• 4 divisions:
• 4 divisions:
–
cecum
–
rectum
–
anal
canal
•
internal
sphincter - smooth muscle
•
external
sphincter - skeletal muscle
•
No
villi or circular folds in mucosa
•
Epithelium
contains mostly absorptive cells (water absorption) and goblet cells (secrete
mucus)
•
Mechanical
digestion
–
Movements
of large intestine begin when substances
pass iliocecal sphincter
•
Haustral
churning
•
distention
of haustra as chyme enters LI initiates haustral churning
•
Peristalsis
occurs at slower rate than in SI
•
Mass
peristalsis
•
Strong
peristaltic wave that begins at mid-transverse colon drives contents into
rectum
•
Occurs during or immediately after meal when food
enters stomach
•
Chemical
digestion
–
Final
stage of digestion occurs in LI through activity of bacteria
•
Produces
gases and other by-products
•
Eg
vitamins
Gut – overview
Gut functions – movement/motility, secretion,
digestion, absorption
•
Digestion and absorption of:
–
Carbohydrates
–
Protein
–
Fat
Gut functions
•
Movement/motility, secretion, digestion
absorption
Movement
•
Propulsion of gut contents from mouth to anus
•
Churning and mixing:
–
Hastens dissolving
–
Emulsification
–
Hastens digestion and absorption
Propulsive movements
•
Rhythmic peristaltic waves along gut
•
Constriction of circular muscles behind food
•
Relaxation in front and contraction of
longitudinal muscles
Sphincters
•
Barriers to movement between parts of the gut:
–
Cardiac – oesophagus to stomach
–
Pyloric – stomach to duodenum
–
Ileocaecal – small to large intestine
–
Internal anal – smooth muscle (reflex)
–
External anal – striated muscle (voluntary
control)
Gut secretions
•
Mucous – protects and lubricates whole gut
•
Saliva, Gastric juice, Bile, Pancreatic juice
& Intestinal juice
•
Total 7L/day
Functions gut secretions
•
Dissolve food – allows taste, makes digestible
•
Emulsifies fat
•
Enzymes to digest food
•
Regulates pH and osmolarity
•
Excretion (bile)
•
Fluid, salts and bile salts all largely
reabsorbed
•
Protein of enzymes – digested and absorbed
Control of gut secretion
•
Cephalic – sight, smell, taste – secretion via
nerve stimulation
•
Receptors in gut (mechanical, chemical or osmotic)
via local nerve plexuses or autonomic reflexes stimulate or inhibit glands
•
Endocrine cells in gut respond to stimuli
release hormone into blood which inhibits or stimulates exocrine glands
Digestion
•
Enzymes in gut secretions break down:
–
Starch and disaccharides to monosaccharides
(only these are absorbed)
–
Protein to amino acids, di&tripeptides (also
absorbed along with tiny amount intact protein)
–
Fat (triacylglycerol) monoacylglycerol and fatty
acids
–
DNA & RNA to free mononucleotides
Absorption
•
Large surface area of small intestine – 600X
that of smooth tube
•
Agitation of gut contents speeds absorption
•
Most absorption in duodenum & jejunum
Carbohydrate digestion
•
In the diet:
–
Sucrose and lactose (disaccharides)
–
Amylose (α1-4 links only)
–
Amylopectin (α1-4 and α1-6
links gives very branched chain and makes up most of starch)
–
Other links e.g. β1-4 in cellulose not broken by digestive enzymes but….
•
α-amylase
in saliva & pancreatic juice:
–
Glucose, sucrose, lactose, maltose, maltotriose
and isomaltose
•
On brush border are specific enzymes maltase,
sucrase, lactase and isomaltase
Carbohydrate absorption
•
Glucose and galactose actively absorbed – this
is a carrier-mediated process and is sodium dependent (linked to Na+
pump)
•
Fructose is carrier mediated but not active.
Facilitated diffusion so relatively slow (also things like sorbitol)
Protein digestion
•
Endopeptidases break bonds within protein chain:
–
Stomach – pepsin
–
Intestine –trypsin and chymotrypsin
•
Exopeptidases break of terminal amino acid:
–
Carboxypeptidase in pancreatic juice
–
Aminopeptidases on brush border
•
A range of di&tripeptidases on brush border
Protein absorption
•
Several active carrier mediated processes, some
are Na+ dependent
•
Some di- & tri-peptides absorbed and
digested within mucosal cells
•
Some intact protein absorbed especially in
newborn by pinocytosis – protein toxins, antibodies and passive immunity
Fat digestion/absorption
•
What is fat – triacylglycerol (TAG)?
•
Actions of lipase in vivo – TAG to
monoacylglycerol and 2 fatty acids
•
Fat insoluble in water but pancreatic lipase is
a water soluble enzyme
•
Fat is emulsified by bile salts and
phospholipids
•
Products of fat digestion also low water
solubility
•
Formation of micelles – minute aggregates bile
salts and fat digestion products
•
Absorption by diffusion
•
TAG re-assembled with mucosal cells
•
Chylomicrons formed and enter lymphatic system
then blood (protein coated fat droplets)
•
Chylomicrons lipoprotein lipase in tissue
capillaries breaks fat down to allow absorption and then re-synthesis of TAG
within cells
The GI Immune System
The digestive system is a potential pathogen portal. Large number of bacteria inhabit the gut 1x10^13. The largest immune 'organ' in the body (GI tract) with specialized structures Gut Associated Lymphoid Tissue (GALT). 80% of all lymphocytes are found in the GALT.
 |
| Immune cells in Preyers Patches |
 |
| Immune cells concentrated in |
 |
| Special epithelial cells called Microfold (M) cells sample the contents of the gut |
If the immune system is activated then immune cells secrete cytokines. Cytokines trigger inflammatory response and increase Cl-, fluid and mucus secretion.
Diarrhea: immune responses can lead to diarrhea which is an attempt to expel the pathogen. Can lead to dehydration
Vomiting: A protective reflex. Reverse peristalsis along with strong muscular contractions
Crohn's Disease





















Great blog! Thank you for sharing.
ReplyDeleteDownload Indian Doctors Network where you can network and communicate with executive committee members, senior doctors and mentors.