What are the different types of hormones? How are hormones released and controlled? What are the major endocrine organs (glands) and endocrine pathogenesis as well as the interactions between hormones (synergistic or antagonistic)
What are hormones?
Hormones: derived from greek verb ormao = 'to excite or arouse', they are chemical messengers secreted into the blood by specialised cells and generally act on remote organ sites and alter rates of processes in target cells. They act at very low concnetrations nano to picomolar range (10^-9 to 10^-12). They control long-term homeostatic processes:Grow, development, metabolism, reproduction and internal environment regulation.
Hormones are produced by endocrine cells and organs - released from endocrine glands. Endocrinology is the study of the endocrine system and hormone action
Hormones act by binding receptors on or in target cells:
- Controlling the rates of enzymatic reactions.
- Controlling the movement of ions or molecules across membranes
- Controlling gene expression and protein synthesis
Hormones have half-lives; i.e. they act for specific period of time before becoming inactivated.
Abit of history of endocrinology:
First experiments performed in mid 1800s. 1849 Berthold and his roosters. 1889 C. Brown-Sequard's Viagra. 1889 discovery of insulin by Minkowski. 1891 thyroid hormone replacement. 1922 purified insulin was used in clinical trials
Types of Hormones
Many different classification schemes:
a. Protein/peptide
b. Steroid (cholesterol derivatives)
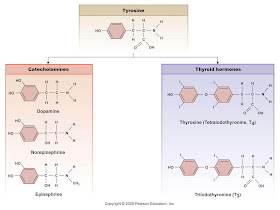
c. Amine (tryptophan or tyrosine derivatives)
OR
i. Lipophilic: penetrate cell membrane readily (steroid hormones and thyroid hormones)
ii. Lipophobic: do not penetrate cell membrane (peptides and catecholamines)
Look at the figure to the right to see the different hormones - must know ALL (espcially the most important - thyroid, parathyroid, adrenal, pancreas, hypothalamus-pituitary, gonads)

A. PROTEIN AND PEPTIDE HORMONES
These are the most common types of hormones.
- preprohormone - large inactive
- prohormone - posttranslational modification
- peptide hormone-receptor complex - signal transduction system
Stored in secretory vesicles and secreted by exocytosis. Dissolved in blood for transport. Act on cell surface receptors - do not penetrate target cell by diffusion.
Rapid onset, short duration and short half-life in the blood - usually inactivated by proteases.
Not active orally. This is because they are proteins/peptides and are digested in the gut (so administration is other than oral cavity - injections!?)
More is discussed below about hormone receptors
B. STEROID HORMONES
- Cholesterol-derived synthesized in the smooth ER. Synthesize as needed from precursors. Lipophilic and can diffuse across membranes and are not stored in secretory cell.
They transported through the blood with carrier proteins. They bind on intracellular receptor (cytoplasmic or nuclear receptors (mostly)) which recognize specific steroids. Steroid hormones induce their effects by altering transcription - they activate or repress gene expression for protein synthesis. They are slower acting and have long duration and longer half-life. May be active orally Examples: cortisol, estrogen, testosterone
 |
| The pineal gland, the thalamus and corpus callosum |
HORMONE RECEPTORS (some things are mentioned below again; this area must be cleaned!)
Hormones work by binding to specific receptors on or in target cells. Receptors are specific for hormone(s). Presence of receptor is necessary for response in cell. Cells have multiple receptors for different hormones. Some hormones have more than one type of receptor; e.g. multiple types adrenergic receptor.
They can get up or down regulation of receptors. Little exposure to hormone - upregulation; e.g. alloxan diabetes. Lot of exposure to a hormone - down regulation - type 2 diabetes?
Agonists: substances that bind to receptor and mimic effect of a hormone. Antagonists are substances that bind to receptor but do not stimulate, so block the effect of a natural hormone. Partial agonists bind and havve low activity, phytoestrogens in soya. Many drugs act as hormone agonists/antagonists
Types of hormone receptors
1. Intracellular receptors that affect mRNA transcription
2. G-protein coupled receptors
3. Tyrosine Kinase associated receptors (RTK)
1. Intracellular receptors
Lipophilic hormone enters cell by simple diffusion. It binds to receptor in nucleus or cytoplasm (translocated to nucleus). Binding induces conformational change and form receptor dimers. The activated receptor has a DNA binding region that binds to ''hormone-responsive elements'' of DNA. Receptor binds to specific base sequences on DNA so affects specific genes. Binding of receptor to DNA switches genes for proteins in that area on or off. Get induction or repression of synthesis of key proteins. Calcitriol (from vitamin D) induces synthesis of several key proteins involved in calcium transport in the gut.
2. G-protein coupled receptors - GPCR
Proteins in membrane with three subunits α,β and γ. They are called G proteins because they are associated with GDP/GTP. G protein complex in membrane with GDP bound to a region. Hormone binds to GPCR increases its affinity for αβγ-trimer. When GPCR and αβγ unit combine, the GDP on the α unit is replaced by GTP. The α unit when bound to GTP dissociates from βγ. The α unit binds to a membrane enzyme (or ion channel) and alters its activity. The α unit is a weak GTPase and as GTP is converted to GDP so it rebinds to form αβγ - so terminating its effects.
G-proteins
There are several types of G-proteins. Proteins Gs and Gi stimulate or inhibit the membrane enzyme adenylate cyclase. This catalyses ATP to cyclic AMP which is a secondary messenger which brings about intracellular hormone effects. There are other second messengers like cGMP, inositol triphosphate, diacyglycerol and calcium.
 |
| Sorry for the informal diagram! |
Glucagon binds to its membrane receptor. The αβγ G protein attaches to the receptor. The α unit's GDP is replaced by GTP; this α unit detaches and binds to and activates membrane adenylate cyclase. Increased cAMP produced inside the cell. α-unit converts GTP to GDP and it rejoins to βγ-unit - cessation of effect. Cyclic AMP binds to and activates cAMP dependent protein kinase (PKA). This protein kinase adds phosphate residues to specific protein sites which activate or inhibit it. Glycogen synthase becomes inactive when phosphorylated - less glycogen synthesis. PKA phosphorylates phosphorylase kinase to make it more active and this in turn phoshorylate phosphorylate b (inactive) to an (active) increased glycogen breakdown. cAMP broken down to AMP by enzyme phosphodiesterase which stops effect. Phosphodiesterase inhibited by caffeine, theophylline and sidenafil (viagra - omg). Phosphatases within cell remove phosphate groups from protein - counteract protein kinases. Enzyme activity depends upon proportion phosphorylated - balance of kinase and phosphatase effects!
cAMP
A number of hormones work via cAMP as a secondary messenger. Precise effect of rise or fall in cAMP depends upon tissue enzymes. Catabolic enzymes are more active when phosphorylated i.e. by increased cAMP - anabolic less active. Theophylline potentiates effects of cAMP and is a derivative of cAMP that penetrates cell and mimics effect of cAMP (hormone?)
Phosphotidyl inositol system
When hormone binds to its receptor it activates a G-protein. The α subunit binds to and activates phospholipase C in membrane. This enzyme converts phospholipid phosphotidyl inositol biphosphate (PIP2) to diacylglycerol (DAG) and inositol triphosphate (IP3) - both are secondary messengers.
Diacylglycerol (DAG)
This activates protein kinase C in the membrane. This causes protein phosphorylation which brings about a response in the cell.
Inositol Triphosphate (IP3)
Enters cytoplasm. Triggers calcium release from endoplasmic reticulum. This calcium binds to a protein called calmodulin which activates a calmodulin sensitive protein kinase. Calcium can also trigger secretion.
Guanylate cyclase
The receptor(s) for atrial natriuretic factor (ANF) have a guanylate cyclase component. The ANF binds to the receptor which increases guanylate cyclase activity. Cyclic GMP is produced in the cell - the secondary messenger.
3. Tyrosine Kinase associated receptors (RTK)
Insulin and receptor tyrosine kinase (RTK)
Insulin receptor is tetramer α2β2. Insulin binds to external binding sites on a subunits. The β subunits are large transmembrane proteins with tyrosine kinase activity. The α units suppress the TK activity but when insulin binds this removes inhibition. The TK units phosphorylate each other and other cellular proteins.
TK effects: activates a protein phosphatase which dephosphorylates glycogen synthase - activated. In cells like muscle and fat releases the glucose transporter GLUT-4 from vesicles to membrane. Other effects also... The hormone receptor complexes aggregate and internalised into vesicles and insulin is degraded.
 | |
| Feedback loop and Response loop |
Afferent: incoming signal: a. Stimulus -> b. Sensor or Receptor -> -> d. Afferent Pathway ->
Efferent: outgoing signal: -> e. Integrated center -> f. Efferent pathway -> g. Target or Effector -> h. Response
(this was the response loop: from stimulus to response)
(Feedback loop: from response back to stimulus is the feedback loop mechanism)......Stimulus -> Sensor or receptor......etc. We gone see how this control mechanism (stimulus then sensor or receptor then afferent pathway to integrated center to efferent pathway then target or effector and response) occurs in other hormones and in different examples. Look (click) at the diagrams!!!
 |
| Example 1 |
 |
| Example 2 |
Major endocrine organs
Brain:
- Hypothalamus (trophic and neurohormones)
- Pituitary Gland (8 major hormones)
Other organ sites:
- Thyroid gland (thyroid hormones and calcitonin)
- Adrenal cortex: cortisol and other steroids
- Adrenal medulla: catecholamines
- Liver: IGFs
- Pancreas: insulin and glucagon
- Gonads: sex hormones
Neurohormone is any hormone synthesized and released by a neuron
Trophic hormone is a hormone that controls the secretion of another hormone.
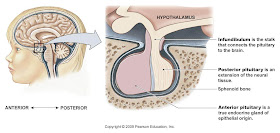
 |
| Posterior Pituitary |
Summary of hormones
Endocrine Control
Three levels:
Hypothalamic stimulation <-- from CNS
Pituitary stimulation <-- from hypothalamic trophic hormones
Endocrine gland stimulation <--from pituitary trophic hormones
What about feedback loops?
 | |
| Example 3 |
 |
| Adrenal Gland: major site of steroid hormone synthesis |


 |
| Other endocrine organs: Thyroid |
Types of Endocrine disorders:
- Hyposecretion: genetic (dwarfism); damage to gland (type 1 diabetes); dietary (thyroid - goiter, low thyroxine); lack of pituitary stimulation
- Hypersecretion:
Genetic (gigantism); overstimulation (hyperthyroidism or overactive pituitary); tumour or cancer; grave's disease or immune mediated
- Abnormal tissue response/Signal transduction abnormalities:
Lack of receptors (testicular feminisation syndrome - mutant adrogen receptor); down regulation receptors (type 2 diabetes); growth hormone abnormalities (mutant GHRH receptor)

Thyrotrophin releasing hormone

Thyrotrophin
Growth Hormone:
 - Growth is a continuous process. In adolescence largest amount of growth in rapid spurts of growth and development. Requires production of other hormones as well as GH. Adequate diet. Abscence of stress i.e. cortisol driven failure to thrive.
- Growth is a continuous process. In adolescence largest amount of growth in rapid spurts of growth and development. Requires production of other hormones as well as GH. Adequate diet. Abscence of stress i.e. cortisol driven failure to thrive.Somatotrophin -------------------->>>

Hormones are synergistic and antagonistic such as the antagonism between insulin and glucagon, thyroid and parathyroid, etc.. The diagram below shows the antagonisms of hormones. Proper balance between them is extremely important for health
Summary:
Hormones are chemical messengers. They are synthesized, released and act at remote sites. Three main groups of hormones (proteins/peptides, steroids, amines). Each group has a different mechanism of action. Hormone release and action is controlled by response feedback loops; these loops can have multiple input and output points. Each endocrine organ makes a specific set of hormones. Hypothalamus and Pituitary gland (hormone central). Steroid hormone synthesis mainly in adrenal gland. Endocrine disorders from hormone imbalances also occur producing hyper/hypo secretion. Like the thyroid gland hyper/hypo, growth hormone production and the pancreas and insulin/glucagon balance. Also remember the importance of hormone synergy and antagonism (look at the hormone wheel diagram!)
--------------------------------------------------------------------------------------------------------------
Now lets talk abit about glucose and calcium metabolism problems
Insulin and Diabetes: An overview
Table of Contents:History and discovery of insulin
Nature of insulin and implications
Actions of insulin
Control of insulin secretion
Glucagon actions
Control of glucagon release
Integrated pancreatic control of blood glucose
Diabetes mellitus and its types
Symptoms and long term complications
Causes
Pathophysiology
Diagnosis
Treatment
Prevention
Introduction
- Islets of Langerhans in pancreas:
α cells secrete glucagon
β cells secrete insulin
- Diabetes mellitus (lack of insulin) most common endocrine disorder
- 1.8 million diabetics in UK (3%) 1.55 million type 2 and may be 1 million more undiagnosed (5% of NHS spending)
- Pima Indians (Arizona) half population over 35 years diabetic - also very prevalent in South Asians in UK.
Historical Landmarks
- 150-200AD term Diabetes (syphon) applied to condition in which ''flesh and bones melt down into urine''
- 1674 the term Mellitus (honeyed) was applied because of urine's sweet taste
- 1889 - Pancreatectomy in dogs produces diabetic-like state postulated that pancreas produces an antidiabetic factor.
- Ligation of pancreatic duct causes degeneration of pancreas but not islets - no diabetes
- 1909 the term insulin was coined but could not be isolated
- 1921 Banting and Best extracted insulin from dog pancreas.
- 1953 Sanger - complete sequence of insulin.1st protein to be sequenced
Nature of Insulin
- Protein hormone of 51 amino acids - not active by mouth. A chain is 21 aa and the B chain is 30 aa. Linkages are S-S links between cysteine residues. Pig and beef insulin are active in humans despite slight differences. First treatments were with impure animal insulin; now use ''monocomponent'' human insulin.
- 1969: Proinsulin extracted from pancreas. Single chain of 84aa and C-peptide (33aa) cut out to leave insulin i.e. 1 gene. C-peptide used as a marker for endogenous insulin production in diabetes.
Actions of Insulin
- Increased synthesis glycogen, fat and protein.
- Increased glucose uptake into muscle and adipose tissue but not brain, liver, red cells, etc.
- Increased glycogen formation and glucose use
- Increased fat synthesis
- Increased protein synthesis in muscle
- Reduced ketone production
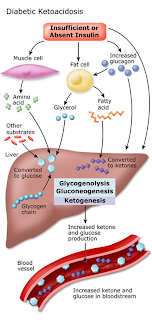
- So lack of insulin.........
Control of insulin secretion
 Increases in blood glucose (and blood amino acids) have direct effect on β-cell. GIP produced by gut in response to eating increases insulin release - anticipatory. Parasympathetic stimulation (vagus) increases release but sympathetic reduces it.
Increases in blood glucose (and blood amino acids) have direct effect on β-cell. GIP produced by gut in response to eating increases insulin release - anticipatory. Parasympathetic stimulation (vagus) increases release but sympathetic reduces it. Glucagon
29 amino acid peptide from α-cells. Increases glycogen breakdown and gluconeogenesis in liver. Release is stimulated by low blood glucose. High blood amino acids increases release but this is suppressed by high blood glucose. Increases by sympathetic or parasympathetic activity,


DIABETES
Diagnosis
- Symptoms plus casual plasma glucose 11.1mmol/l.
- Fasting (8h+) plasma glucose 7.0mmol/l (6.1 for whole blood).
- 2h plasma glucose 11.1mmol/l during oral glucose (75g) tolerance test.
- 6.1-7mmol fasting impaired - half will become diabetic within 10yrs
- No symptoms - need to repeat
 |
| Type 1 diabetes |
- Less than 10% of total
- Characterized by β-cell destruction and almost total failure of insulin supply. Fairly rapid onset usually in childhood. Need isnulin injections and prone to ketoacidosis
- Often thin at diagnosis. Inherited predisposition (linked to tissue-type) - environmental trigger(s) e.g. infection
- Most have autoantibodies to β-cells at diagnosis
Type 2 diabetes
 |
| Type 2 Diabetes |
- Usually overweight at diagnosis
- Symptoms relatively mild at start and ketoacidosis uncommon (undiagnosed)
- Most do not need insulin unless advanced
- Runs in families but not linked to tissue type and no islet cell antibodies present
- Prevalence increasing as population ages and gets fatter
 Causes of type 2 diabetes:
Causes of type 2 diabetes:- No initial β-cell pathology and insulin still produced (absolute level may be high)
- Reduced sensitivity to insulin - need more to get same effect
- Genetic susceptibility - racial differences
- Environmental triggers - ''western diet and lifestyle''
high fat diet; inactivity; overweight and abdominal obesity
Metabolic syndrome (syndrome X)
- Insulin resistance causes problems even without diabetes: high blood insulin, moderate hyperglycaemia, hypertension, raised blood TAg and lowered HDL.
- Many later become diabetic and all at increased risk of CHD
Diagnosis
High waist (102cm men or 88cm women)
or WHR 0.95/0.85
Moderate fasting hyperglycaemia
Elevated BP
Elevated TAG
Low HDL
ANY THREE suggests diagnosis
 | |
| Symptoms of Diabetes Mellitus |
Symptoms of
diabetes mellitus
High blood glucose (diagnosis) –
why??
Glucose in urine – why??
Diuresis – why??
Prone to dehydration despite
increased thirst and drinking
In type 1 get ketoacidosis:
Fatty acids →Acetyl CoA → Ketones
Rapid weight loss (may also occur in
type 2 so underestimate link with obesity)
Hypoglycaemic coma?
Diabetics tend to die prematurely
despite effective short term treatment
Very high rates of cardiovascular
disease – insulin resistance (pre-diabetes) is a risk factor for heart disease
Also prone to retinopathy and
cataracts – blindness
Diabetic nephropathy (renal failure)
Gangrene and risk of amputation
High levels of blood lipoproteins causing increased risk of
atherosclerosis in arteries
Changes in functioning of small blood vessels due to persistent
hyperglycaemia and glycosylation of protein in membranes
Latter thought to be important factor in retinopathy and renal failure
To improve
long term prospects
Normalise blood lipoprotein profile
Normalise body weight
Minimise the hyperglycaemia without
repeated bouts of hypoglycaemia
Diagnose and treat hidden cases
because long term damage is ongoing
Implementation
Low (saturated) fat diet – prior to
1970 diabetic diet was high fat low carbohydrate. sSubstitution of complex for
simple carbohydrates, increase in dietary fibre, restriction of energy intake
(when necessary)
This helps to normalise blood
lipoproteins but also improves insulin sensitivity
Rapid self monitoring of blood
glucose
Long term check – glycosylated
haemoglobin
Use of rapid soluble insulin and
prolonged action depot insulin
Oral
hypoglycaemic agents
Sulponylureas act to stimulate
insulin release (e.g. tolbutamide and chlorpropamide) – only work in type 2
where there are functioning β-cells
Biguanides – reduces hepatic
gluconeogenesis, slows absorption from gut and increases uptake by muscle
2 Trials
Diabetes Control and Complications
Trial DCCT) for type 1
UK Prospective Diabetes Survey - type
2
Development renal, retinal &
neuropathy delayed by intensified therapy
Higher glycated Hb – more
complications & deaths
Calcium and Osteo
Calcium Balance
- Overview of typical calcium fluxes
- Vitamin D – nature and role
- Role of parathyroid hormone
- Role of calcitonin
- Integrated control of blood calcium
- Osteoporosis
- What is it?
- What causes it?
- What can be done about it?
Calcium
For adults:
Gains – losses = 0
Growth & pregnancy – net gain
Gains and losses hormonally
controlled
99% of body calcium is in bone
mineral as hydroxyapatite – c1kg
Bone is a reserve of calcium –
release or uptake of Ca2+ hormonally controlled
Muscle contraction – excitation
triggers Ca2+ release which triggers contraction
Hormone/transmitter release
Intracellular regulator
Co-enzyme function – blood clotting
Etc
So blood calcium finely regulated and
must be kept within narrow limits
Osteoporosis
Thinning of bones making them
susceptible to fracture e.g. from simple fall
Up to 3 million people in UK may be
affected – annual toll of:
70,000 hip fractures
40,000 recorded vertebral fractires
50,000 wrist fractures
c20,000 death each year attributable
to hip fractures
Nature of
osteoporosis
Osteoclasts – breakdown of bone
Osteoblasts – make new bone
Bone constantly being remodelled but
in later life synthesis slightly less than breakdown so gradual erosion
Risk factors
for osteoporosis
Bone mass declines with age
acceleration at menopause (more elderly women more osteoporosis)
Inactivity – weight bearing exercise
increases bone mass and inactivity leads to loss of bone
Lack of sex hormones (even in men)–
early menopause, anorexia etc
Lack of vitamin D (sunlight exposure)
What about calcium intake??
Smoking, heavy drinking, being
underweight
Osteoporosis
– strategies for reducing its effects
Increase peak bone mass – e.g.
encourage activity in children and young adults
Slow decline in bone mass – activity,
vitamin D, HRT in older people also drugs that block bone breakdown
Reduce risk of falling – building
design and maintenance, maintain muscle strength, protect hips with padding?
Increase bone strength – reverse
process of oseoporosis
Conventional
treatments
Oestrogen therapy – good preventative
Vitamin D/calcium - 40% of old people
in residential homes have biochemical evidence of vit. D deficiency
Calcitonin as nasal spray or by
injection – blocks bone breakdown
Biphosphonates are analogues of
pyrophosphate (etidronate and alendronate) adsorbed onto bone mineral and
inhibit resorption
Teriparatide
– new treatment
Active parathyroid analogue which is
injected
Leads to formation of strong new bone
– reverses osteoporosis
Treatment for up to 18 months and
benefits last beyond this
Theory:
Pth leads to increased renal Ca2+
reabsorption, vit D activation and bone breakdown – but latter only at high
doses
At low doses Pth stimulates
osteoblasts (bone makers) before osteoclasts (bone breakers)
HRT
HRT has been first line preventative
for osteoporosis
Endometrial cancer is a clear risk of
oestrogen alone so must give with synthetic progestin if uterus present
Conclusively show to reduce bone loss
in postmenopausal women
Case-control studies – up to 50%
reduction in hip fractures in menopausal women taking oestrogen
More
problems with HRT
Nelson et al (2002) – HRT increased
risk of heart disease in elderly women
Beral et al (2003) Million women
study – HRT small increase in breast cancer risk
2003 MHRA advised GPs that HRT should
not be used for long periods to prevent osteoporosis in women over 50
Phyto-oestrogens
Are these an alternative to HRT?
Substances from plants not steroids
but have oestrogenic activity
Isoflavins (genistein, daidzein) from
soy and other legumes
Lignans in whole grains
Coumestins in clover and alfalfa
sprouts
Soy foods and supplements, blach
cohosh, red clover
2-4 mg isoflavins per mg soy protein
Supplements c40mg/day
Some diets high in soy 100mg/day
Babies soy formula 4mg/kg body weight
Act as partial agonists so can
increase or decrease oestrogenic activity depending upon circumstances
c1:10,000 potency of oestrogen
But HRT c50μg/day whereas supps 1000X more by weight
of isoflavins
So significant total activity
Branca 2003
In vitro genistein reduces osteoclast
activity but increases osteoblasts
Soybean feeding increases bone
density in ovariectomised rats
Women in SE Asia (where soy intakes
are high) – women with highest intakes have higher bone density
Not seen where soy intakes are lower
(need high dose)
Review of 7 studies suggest
phyto-oestrogens over 6 months positive influence on bone density in lumbar
spine
Phyto-oestrogens – substantial report
published by Food Standards Agency
Other benefits?
Possible risks?
































It's a great share about harmones.
ReplyDeletecomprar DHEA 25mg
Supplementing vitamins and antioxidants can provide superior natural antioxidant protection than diet alone. wildrose detox
ReplyDeleteFor any endocrine related problems consult the best Endocrinologist in Kochi
ReplyDeleteWell written article. Get rid of the traditional ways of marketing and buy a customized email list from us. One real-time data can change your entire business for good. Parana Impact provides you the Email List that you are exactly looking for.
ReplyDeleteWe have worked with many organizations of all the sizes. Our main focus is customer satisfaction. Endocrinologist Users Email List
Got to learn a lot of things from this article. It can be used for any kind of business. Pegasi Media Group the world's leading database vendor and the most preferred organization all over the globe. Our brand is well-known in the market. The organizations of all the sizes have experienced our services and are quite pleased with it. We perform the activities like data cleansing, data appending, data updating, data validation, and data verification on a regular basis before the final delivery. You have also got the tremendous flexibility to choose the geographical location and reach out to the prospects that you target.Endocrinology Email List
ReplyDeleteVery impressive article! The blog is highly informative and has answered all my questions.
ReplyDeleteTo introduce about our company and the activities, B2B contactlist
is a database provider that helps you to boost your sales & grow your business through well-build Endocrinology physicians mailing lists.
Irrespective of receiving daily oral or future in jectable depot therapies, these require health care visits for medication and monitoring of safety and response. If patients are treated early enough, before a lot of immune system damage has occurred, life expectancy is close to normal, as long as they remain on successful treatment. However, when patients stop therapy, virus rebounds to high levels in most patients, sometimes associated with severe illness because I have gone through this and even an increased risk of death. The aim of “cure”is ongoing but I still do believe my government made millions of ARV drugs instead of finding a cure. for ongoing therapy and monitoring. ARV alone cannot cure HIV as among the cells that are infected are very long-living CD4 memory cells and possibly other cells that act as long-term reservoirs. HIV can hide in these cells without being detected by the body’s immune system. Therefore even when ART completely blocks subsequent rounds of infection of cells, reservoirs that have been infected before therapy initiation persist and from these reservoirs HIV rebounds if therapy is stopped. “Cure” could either mean an eradication cure, which means to completely rid the body of reservoir virus or a functional HIV cure, where HIV may remain in reservoir cells but rebound to high levels is prevented after therapy interruption.Dr JAMES Herbal Medicine makes me believes there is a hope for people suffering from ACUTE MYELOFIBROSIS, ALZHEIMER's symptoms, BREAST CANCER, DIABETES, HAIR LOSS AND HAIR TREATMENT, KIDNEY DISEASES, LEUKEMIA, MYELOID LEUKEMIA, STEM CELL TREATMENT,Parkinson's disease,Schizophrenia,Cancer,Scoliosis,Fibromyalgia,Fluoroquinolone Toxicity
ReplyDeleteSyndrome Fibrodysplasia Ossificans Progressiva.Fatal Familial Insomnia Factor V Leiden Mutation ,Epilepsy Dupuytren's disease,Desmoplastic small-round-cell tumor Diabetes ,CARDIAC disease,Creutzfeldt–Jakob disease,Cerebral Amyloid Angiopathy, Ataxia,Arthritis,Amyotrophic Lateral Sclerosis,Alzheimer's disease,Adrenocortical carcinoma.Asthma,Allergic disease HIV & Aids,Herpes ,Copd,Diabetes,Hepatitis,I red about him online how he cured Tasha and Tara so I contacted him on >drjamesherbalmix@gmail.com< even talked on >whatsapps +2348152855846< believe me it was easy I drank his herbal medicine for two weeks and I was cured just like that isn't Dr James a wonder man? Yes he is! I thank him so much so I will advise if you are suffering from one of those diseases. Please do contact him and get permanent treatment with his powerful herbal mix now he's a good man.
Hello,
ReplyDeleteI liked your blog very much it is very interesting and I learned many things from this blog which is helping me a lot.
Thanks a lot!
Top Thyroid Doctors In Chennai
Great blog! Thank you for sharing.
ReplyDeleteDownload Indian Doctors Network where you can network and communicate with executive committee members, senior doctors and mentors.
Amazing Blog Post about Endocrinolgy harmones Please Update Latest Treatment and procedure.
ReplyDeleteFor Houston endocrinology Book Online and infront Appointment now.
I liked it and enjoyed reading it. Keep sharing such important post. Apart from this you should read this How Hormones Affect Weight Loss article. This time of year I tend to start hearing more and more about difficult weight loss. Individuals that have worked hard over the last few months to lose that extra winter weight are finding that despite the fact their diet has changed drastically, and they are incorporating exercise into their daily routine, they are at a stand still, simply unable to lose any extra pounds. For more information Check out this How Hormones Affect Weight Loss article.
ReplyDelete